
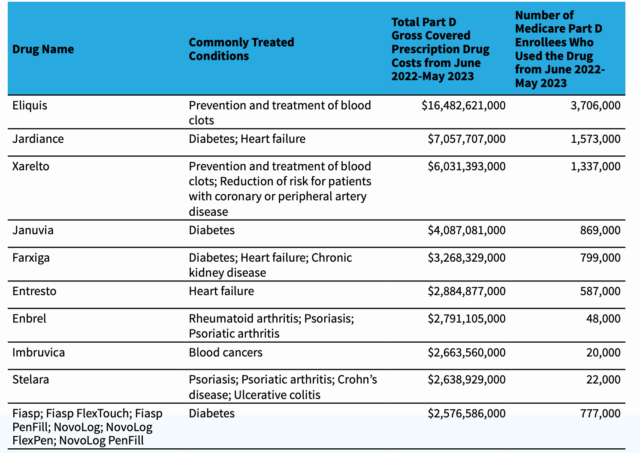
Starting January 1, 2026, pharmacies will be reimbursed under a different model for dispensing certain Part D Medicare drugs. These changes are a part of the implementation of the Inflation Reduction Act of 2022 (P.L. 117-169), which provides Medicare the ability to directly negotiate the prices of certain high expenditure, single source drugs without generic or biosimilar competition. The Centers for Medicare & Medicaid Services (CMS) selected ten drugs covered under Medicare Part D for the first cycle of negotiations for initial price applicability year 2026:
Source: https://www.cms.gov/files/document/fact-sheet-medicare-selected-drug-negotiation-list-ipay-2026.pdf
It is imperative for pharmacies to understand how they will be paid for these drugs and to navigate any cash flow risks that this new reimbursement model brings.
For many years, I have been working with “Family Owned Pharmacies” consultants, who are at the forefront of the changes and issues that independent pharmacies face. Jerry Josephson and Richard Diamond provide tremendous resources and are big advocates of independent pharmacies. This time, they have prepared an excellent overview of the upcoming Part D changes and a roadmap for independent pharmacies to follow. If you own an independent pharmacy, I strongly recommend reviewing these two documents and sharing them with your staff.
The first document “MFP Explained” explains the program, practical risks, cash flow issues, and what you should do to minimize them.
The second document “Practical Implications” provides valuable tips on how to flag these claims, adjust your workflow and provides a specific script to send to your pharmacy software vendor.
Hope you find these resources valuable and practical. And if you do, feel free to reach out to Richard and Jerry at “Family Owned Pharmacies” and sign up for their free RxOwnerAlerts by emailing Jerry at: jjosephson@ultimabsc.com.
